Thousands of Doctors in England Refuse to Work, Sparking Healthcare Crisis
England's Junior Doctors Launch Five-Day Strike Over Pay Erosion That Has Left Medical Assistants Earning More Than Qualified Physicians
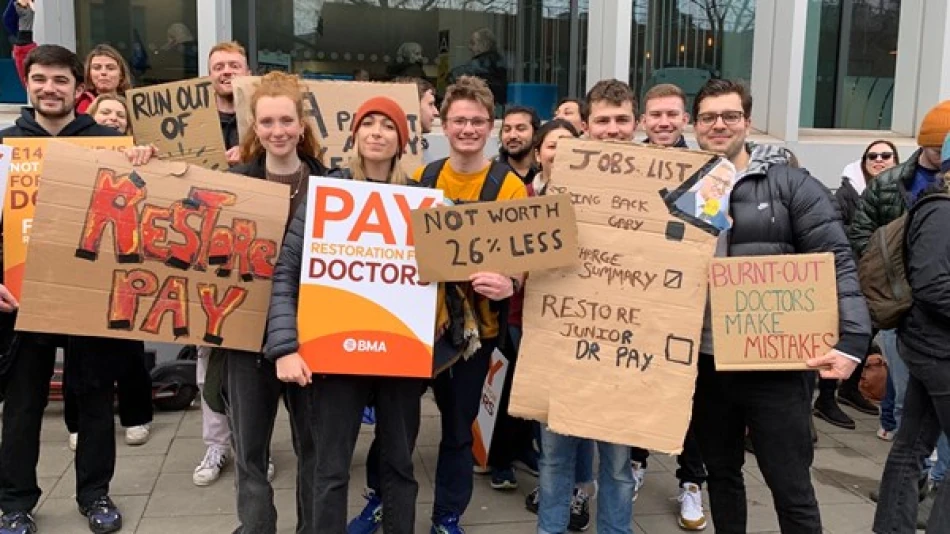
Thousands of junior doctors across England's state-funded National Health Service have begun a five-day strike over pay disputes, highlighting a deepening crisis where qualified physicians now earn 30% less than medical assistants in some cases. The walkout, which started Friday, threatens to disrupt patient care nationwide as salary erosion since 2008 has reached a breaking point that unions say undermines the entire healthcare system.
The Pay Inversion Crisis
The strike centers on a stark reality that would have seemed impossible a generation ago: medical assistants in some NHS trusts now earn more than qualified junior doctors. According to the British Medical Association (BMA), junior doctors have experienced a 20% real-terms pay cut since 2008 when inflation is factored in, creating an inverted wage structure that defies medical hierarchy and training investment.
Dr. Melissa Ryan and Dr. Ross Newwood, co-chairs of the BMA's junior doctors committee, emphasized that "salary erosion has reached the point where a physician assistant's salary can exceed that of a junior doctor by 30%." This wage inversion represents more than just a pay dispute—it signals a fundamental breakdown in how England values medical expertise and training.
Healthcare System Under Strain
Junior doctors, who form the backbone of hospital and clinic operations despite being early in their careers, have positioned themselves outside hospitals in protest after negotiations with the government collapsed. The NHS has assured that emergency departments will remain open and hospitals will attempt to provide care for as many scheduled patients as possible, but the five-day duration suggests significant service disruption.
Broader Implications for Medical Recruitment
The pay structure crisis extends beyond immediate patient care concerns. When qualified doctors earn less than support staff, it creates perverse incentives that could drive medical talent abroad or into private practice. Countries like Australia, Canada, and Germany have actively recruited British-trained doctors with competitive salary packages, making the UK's pay stagnation a national competitiveness issue.
Government's Difficult Position
The government faces a complex balancing act between fiscal constraints and maintaining healthcare quality. Public sector pay restraint has been a cornerstone of economic policy since the 2008 financial crisis, but the healthcare sector's unique training requirements and social importance make it particularly sensitive to wage compression.
Unlike other public sector disputes, medical strikes carry immediate public health implications and generate significant political pressure. The five-day duration suggests junior doctors are prepared for a prolonged confrontation, potentially forcing the government to choose between budget discipline and healthcare system stability.
International Context and Lessons
England's healthcare pay crisis mirrors broader trends in public healthcare systems globally, but the severity of wage inversion appears particularly acute. France and Germany have maintained more competitive medical salaries relative to support staff, while countries like New Zealand and Australia have used targeted recruitment campaigns to attract British medical talent.
The strike represents a critical test case for post-pandemic healthcare policy. If successful, it could trigger similar actions across other UK regions and potentially influence medical pay structures throughout Europe's public healthcare systems.
Most Viewed News

 Layla Al Mansoori
Layla Al Mansoori






